After altering his looks and taking psychiatric lessons every day for one week, investigative journalist ‘FISAYO SOYOMBO went under cover for three weeks in November, including 10 straight days on ward admission, as a patient of the Federal Neuropsychiatric Hospital, Yaba, Lagos, one of the nation’s most historic mental rehabilitation centres. His report unveils the decrepit state of hospital facilities, gross shortage of critical staff despite a bloated workforce widely believed to be populated by ghost workers, low quality of service delivery, arbitrary charges on patients — all stemming from personal and institutional corruption and the hospital’s implicit stigmatizing of its very own patients.
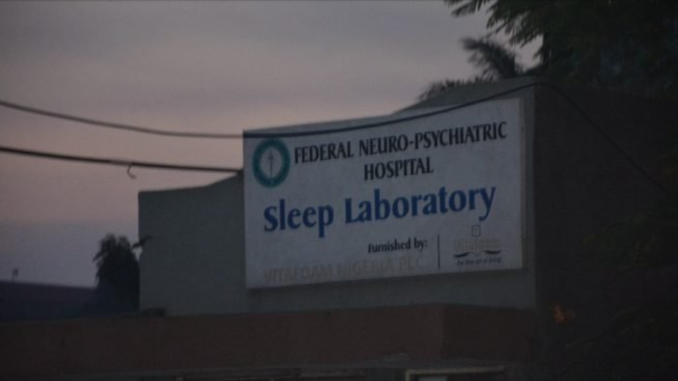
We believed we had missed our way that sweltering afternoon of Tuesday November 12, 2019, when we prematurely turned off Harvey Road into a building we were half sure was the Federal Neuropsychiatric Hospital, Yaba, Lagos. But we were less than five seconds in when we knew we were indeed at ‘Yaba Left’, as the hospital is colloquially, and more popularly, known.
“We’re going to the psychiatric hospital; are we in the right place, please?” I asked the gatekeeper as politely as I could. To my utter shock, he flared up. “You are at Yaba Left and you’re still asking again,” he screamed. “Oga, you wan enter or you wan comot?”
In truth, we had expected this sort of aggressive behaviour. This, after all, was a hospital for treating the mentally ill. We just didn’t expect it so soon.
IN THE BEGINNING

The history of mental rehabilitation in Nigeria is incomplete without the Neuropsychiatric Hospital, Yaba, Lagos. Since beginning life as the Yaba Lunatic Asylum in October 1907, when its primary purpose was to serve as a holding place for keeping the mentally ill out of the way of ‘normal’ people in the society, the hospital has played a leading role in the evolution of mental care to treatment and healing, not just holding, of patients.
In the opening years of its founding, and until 1950, it was purely an asylum. The first batch of 48 inmates were admitted in a rundown Nigeria Railway Building in Yaba. It was a time West Africa was generally witnessing the opening of asylums. Before this time, the mentally ill were kept in the custody of native doctors, who often contained but sometimes restrained them.
By 1951, qualified psychiatrists, nurses and pharmacists were starting to arrive. After it was managed by expatriates until the mid-1950s, the responsibility of management fell on Abraham Ordia, the first Nigerian psychiatric nurse. The next 20 years would witness the creation of an outpatient department and the commencement of occupational therapy. From the Yaba Asylum, it became the Yaba Mental Hospital. These changes were accompanied by a rising patient population that wasn’t matched by increased staffing. One hundred patients in 1925 became 200 in 1944 and 448 in 1961, yet only one doctor manned the facility. It wasn’t until 1961 that two more psychiatrists — Dr. A Boroffka, a German, and Dr. A Marinho, the first Nigerian psychiatrist to work at the hospital — were employed.
More recent decades have seen the staffing of nurses and pharmacists, a second name change to the Neuropsychiatric Hospital and the appointment of Nigeria’s first female psychiatrist as Chief Medical Director (CMD) of the hospital. These strides notwithstanding, Yaba Left was neck deep into violating is ‘guiding principles’, listed on its official website to include “patient-centred service delivery, patient and staff welfare, transparency and accountability”.
THE DELICATE JOURNEY TO YABA LEFT

After three unrelated complaints in two years about the standard of medical services on offer, I decided to experience the hospital myself as a patient rather than believe the complainants. To help devise a medically impregnable entry strategy, I enlisted the services of a US-based mental health expert. When we communicated for the first time in the first week of October, he explained I could only enter as a drug addict requiring rehabilitation after abusing marijuana and cocaine. If I faked the regular, mentally-ill patient, I would definitely be found out, he explained.
“That means I have to ingest cocaine just before I go in?” I asked. With the benefit of hindsight, I was only displaying the naivety that made me know I had to contract him in the first place.
“Not on your life!” he warned. “Close your eyes. Imagine yourself having sex and you’re just about to climax.”
Silence.
“You see that feeling, cocaine will give you five times of it. Cocaine addiction, if it happens, is almost impossible to solve. You should never touch cocaine for any reason. Never.”

This small mass of crack cocaine — worth between N5,000 and N10,000 depending on location of purchase — will ruin your life. Flee from it!
We agreed I would take no drug, not even marijuana. However, I would be taught how to answer a doctor’s questions like a drug addict. He told me that on arrival at Yaba Left, I would be grilled by a doctor for roughly three hours. I had to answer the questions in such a manner to make my addiction serious enough for hospital admission yet unserious enough for injection or drugs. Tough one. One mis-answered question could convince the doctor that I was unworthy of admission, which would spell the end of the story or, worse still, I could be admitted but placed on drugs/injection, which will subject me to some unpleasant side effects.

Crack cocaine… Many Yaba Left patients genuinely want to quit but it looks beyond them. Best is never to try.
One more warning: no patient admitted at Yaba Left could refuse drugs or injections; any patient who tries it would be forcefully subdued by the Crisis Intervention Personnel, famed within and beyond the hospital for their reputation to overpower the hardest of drug addicts and mentally-ill patients. My mental health expert and I knew the three-hour questioning was crucial; for this reason, we held six virtual meetings in late October — three for learning the answers to the questions and another three for reenacting the sessions. After making a few alterations to my looks, I presented myself to doctors at the Neuropsychiatric Hospital, Yaba, as a drug addict in need of rehabilitation, just like any other member of the society. My discoveries were disturbing.
BED-SPACE CORRUPTION
Even though Dr. Akingbola, as I later found her name to be, was evidently in the third trimester of her pregnancy, she proved herself a class act, professionally. Dressed in a loose pair of black trousers and a flowing, silky robe, she stood up when she needed to, talked when she should, listened when she should, despite battling personal discomforts that manifested in the form of repeated sneezes and coughs. Dr. Akingbola did not speed up the questioning one notch; it lasted nearly the full three hours I’d anticipated. Her overall professional conduct was impeccable.
A consultant whose name I later established to be Dr. Ogunlowo courteously interrupted us from time to time, interacting with the first doctor in a manner suggesting he was trying to help her settle. I easily concluded Dr. Akingbola was either newly employed or relieving another doctor at the hospital. A consummate professional, Dr. Ogunlowo’s face lit up with glee once Dr. Akingbola announced to him that I voluntarily walked in; medically, I was “motivated”. Motivation, I’d been pre-informed, is big deal to psychiatric doctors. Motivated drug patients stand a better stead of overcoming their psychiatric disorders than those coerced or bundled into the facility. Dr. Ogunlowo couldn’t hide his excitement. But there was a little problem.
“There’s no bed space,” he announced to me.
I couldn’t believe my ears. This, coupled with its annex at Oshodi, is the only Federal Government-owned full-fledged psychiatric hospital serving the whole of Lagos — Nigeria’s ex-seat of federal power, most populated state, current economic capital — and only one of two available in the six states of the South West. It is also one of only eight public psychiatric hospitals serving an estimated 200 million Nigerians, one of every eight of whom were long proven by the World Health Organisation (WHO) to be suffering from one form of mental illness or the other. It’s a 535-bed facility; however, only two male wards comprising 60 bed spaces and a female ward of 30 bed spaces were wholly dedicated to drug patients.
“Don’t worry; come back next week. I’ll keep a space for you,” Dr. Ogunlowo’s words interjected my thoughts. “I don’t usually do this, but I see you’re motivated, and I don’t want you to go back to drugs.”
Going back to drugs was not the problem; it was that I’d already altered my looks; I couldn’t move about this way, yet I wasn’t prepared to be idle indoors. Having told them minutes earlier that I came in from Ibadan, I begged them not to allow me go. “Please help me,” I pleaded soberly. “If I go back to Ibadan, I may not come back.”
Actually, this is the reality of real drug addicts; they hardly reach a point where they opt for admission, and if they ever do, only to get turned back, it’s bye to the hospital and back to the lure of drugs. Days later, I would overhear a doctor lamenting to a colleague about a young female crack cocaine addict who found time out of her banking job to seek help at the hospital; unfortunately, it was one of those numerous no-bed-space days. The doctor exchanged contacts with the lady, promising to alert her once a space opened up. Space opened up two weeks later but the banker never returned. It’s 18 months after but the doctor hasn’t quite managed to convince the lady to come back! If I was indeed a drug addict, the system had failed me.
Unlike the regular cocaine, crack is far more potent and addictive. Because it is smoked (rather than snorted through the nose), the drug reaches the brain more quickly, producing an intense and immediate ‘high’, which, it must also be said, is short-lived. Since the ‘high’ experienced by abusers is so pleasurable even if ephemeral, they constantly need more of the drug to maintain it. Eventually, an addiction is born, and the user needs the drug to simply feel normal. I begged doctors Ogunlowo and Akingbola profusely, but there was no reprieve. I could tell that the two doctors genuinely felt helpless.
One member of my team approached an official of the Crisis Intervention Personnel for help. I had been told that the ‘Crisis’, as they were simply called, sometimes pressured doctors into taking patients in. Olaniyi Olawale pressed for hours but didn’t succeed. Before we left the hospital a little past 9pm, we greased his hands with N5,000 — to say thanks for his effort. At that point, it was an honest gift from us; not a bribe. Soon, Olawale would prove himself a member of a syndicate at the hospital that specialized in arranging bed space for under-pressure patients in exchange for a token, often at the expense of more deserving patients.
Realising, shortly before leaving, that he hadn’t collected Olawale’s number, a member of my team approached a hospital orderly, Mrs. Adeniyi, for Olawale’s number. Mrs. Adeniyi declined to release it, instead insisting that we talk to her.
“Do you want to give him something?” she queried knowingly, furtively flickering her eyes over each one of us. “What exactly do you want? Talk to me.”
Mrs. Adeniyi assured us she could secure bed space for us, but she made it clear we would need to “settle”. To prove our seriousness, we handed her N2,000 and collected her number. To protect her own interest, Mrs. Adeniyi refused to release Olawale’s number even though she had it. Well, we found it through alternative means the following day, Wednesday November 13, and contacted him.
N10,000 OR N7,000, BED SPACE AT YABA LEFT ‘DOESN’T COME FREE’
On Thursday, Olawale’s call was what roused me from sleep. He had found a hospital staffer by the name Tosin Karunwi, who was willing to secure bed space for me, provided we understood that “nothing comes free”. We weren’t sure if Karunwi was a nurse, an orderly or a Crisis official, but we established that she indeed worked at the hospital.
Olawale announced that Tosin had demanded N10,000 to help lock down a bed space for me, but he successfully negotiated a N7,000 deal. He asked us to forward the money to Account Name ‘Olaniyi Olawale Matthew’ with Access Bank — because Tosin didn’t want the money sent to her. He passed the money on to Tosin, after she agreed to return it if she didn’t secure a bed space.
To our utmost shock, once she took possession of the money, Tosin began to sell Oshodi to us. Actually, Oshodi, the neuropsychiatric hospital’s annexe, was even worse managed than Yaba. It was graveyard-like, largely abandoned. Oshodi was technically the hospital into which Yaba’s vomits were spilled. But Tosin argued otherwise.
“Wait a minute, why don’t you want Oshodi?” she’d asked on phone in the evening of Thursday November 14. “Oshodi and Yaba are the same. Three bed spaces are vacant at Oshodi; I’d advise you to take one of them.”
On December 3, three full weeks after Tosin was paid for the bed space that never came, she was told to refund the payment, but she refused, and blatantly too. “You cannot get N7,000,” she snapped. “The [two] nurses I gave money to, do you expect me to pay back on their behalf? Maybe I can send N4,000 to you; it’s just maybe. Maybe. That’s even if I’m able to raise it. Do you expect me to hold the cash or keep it in the bank?”
Tosin claimed that no space had opened up at all, both at Yaba and Oshodi “since last week”. What she didn’t know was that I’d gone in (and come out) as a patient because a space indeed opened up for me, and that at least two more opened up during my stay.
‘YABA LEFT ANNEXE DOESN’T HAVE A GOOD DRUG REHABILITATION PROGRAMME’

Inside this gate, at Oshodi, is the annexe of the Federal Neuropsychiatric Hospital, looking not one bit like a hospital
Some days after I started discussing admission with Olawale without success, I returned to Yaba to try to force the issue. There, I met a doctor who surprisingly urged me not to waste my money on admission at Oshodi. Instead, this doctor advised me to consider the Federal Neuropsychiatric Hospital, Aro, Abeokuta.
“The issue is this: at Oshodi, you may not get the maximum benefit you need, to be sincere with you,” the doctor said. “I work here, and I know that after a while you may be frustrated, because what you will be doing there is not really rehabilitation. Many of the patients at Oshodi are psychotic; they have one form of behavioural disorder or the other. The hospital’s programme for rehabilitation is not well-developed over there, so you may be there for days without seeing a psychologist.”
When I insisted I’d rather take Oshodi than wait endlessly for bed space to open up at Yaba, the doctor replied: “Probably it’s because you don’t know how Oshodi is.”
This was the same Oshodi that Tosin was trying to trick me into accepting admission at.
THE ORDERLIES ARE CORRUPT — BRAZENLY SO

Mrs Adeniyi, one of the shady orderlies who have devised numerous ways of swindling patients of their money.
For the fourth time in less than a week, I was back at the Neuropsychiatric Hospital, Yaba, on November 18 without any assurance of securing bed space. After more than six hours of laborious wait, intense lobbying to see doctors and queuing up to pay fees, my admission was finally confirmed.
“Bring N20,000,” Mrs. Adeniyi, the orderly, ordered right inside the hospital reception. She never told us what it was for, and we got no receipt after paying. We would later find out it was for a Ghana-Must-Go bag I was to enter the ward with. The contents were a 400g sachet of powdered Dano milk, a 500g sachet of Milo chocolate and malt powder, two pairs of velvety pyjamas that threatened to tear up at the slightest pull, a medium-size towel, a small takeaway-style food plastic, a 140g package of CloseUp tooth paste, a stick of Oral tooth brush, a small-size cup, Two 65g bars of Premier Cool soap, two pairs of plastic spoon, two pairs of boxer briefs, one low-grade round-necked vest and a sachet of little-known detergent. It wasn’t until I arrived at the ward that I discovered other patients had been similarly swindled. The contents of the bag shouldn’t even cost up to N15,000. Securing bed space at Yaba Left is so difficult that those who finally succeed are too physically and psychologically exhausted to ask too many probing questions before complying with payment instructions.
AN INTRODUCTION TO THE WORLD OF YABA LEFT’S UNBELIEVABLY BIG RATS
I arrived at Tolani Asuni, one of only two male drug wards at Yaba Left, in a hospital ambulance some minutes past 5pm. It was a block of five rooms comprising six beds each. Thirty patients in all. Opposite it stood Adeoye Lambo, similar in number of rooms and bed space, but spotting a major difference that will be discussed later. The two wards are named after perhaps the two most influential Nigerian psychiatrists ever, both deceased. While Professor Thomas Adeoye Lambo, who died in 2004 aged 80, was Nigeria’s and Africa’s first-ever western-trained psychiatrist and a former Vice Director-General at the World Health Organisation (WHO), Professor Tolani Asuni, aged 87 when he died in 2011, is remembered till date for his wide-ranging scholarly and leadership contributions to psychiatry in Africa. It was Lambo, in fact, who, in 1956, convinced Asuni to take up psychiatric training. Till date, Lambo is remembered as a world leader and one of the first to promote psychosocial rehabilitation for persons with mental illness and disability, and to develop primary care in the community for persons with mental illness in Africa. Fitting, therefore, that the wards named after both men at Yaba Left stood opposite each other.
Dinner, served every 6pm, was eba and egusi, but I waited until a little after 8pm before eating. It was the first time in decades I was seeing eba so full of lumps, and egusi so bland and watery. Even though I had not eaten all day, I lost my appetite instantly. I had ingested no more than three morsels when I spotted a strand of local sponge in the egusi. I showed my ‘neighbour’.
“Welcome to Yaba Left,” he exclaimed.
I tucked it away quietly under my bed, just beside one of the four iron poles anchoring the bedframe. The plan was to lodge a complaint with the nurses the following morning. How wrong I was! By 7am the next day when I checked, the strand of sponge was gone.
“Anything you don’t want rats to touch, don’t put it on the floor,” a patient announced to me when I moaned aloud. “Even your Ghana-Must-Go bag. Everything you have should be on your bed!”
I would learn about Yaba Left rats in the evening of my second day at the ward. Well-fed and therefore robust, they roamed the greenery separating Tolani Asuni from Adeoye Lambo in their droves every night. Not that I hadn’t seen rats before, I just didn’t know rats so big existed anywhere in the world.
“It’s been brought to the attention of the Chief Medical Director several times, but she said there’s nothing wrong with it,” one patient told me.
Actually, many things are wrong with the population of rats inside Yaba left. Lassa fever, a viral infection caused by the Lassa fever virus, is, for example, primarily transmitted to humans via contact with excreta from rats. According to the Nigeria Centre for Disease Control (NCDC), Lassa fever is spread through “direct contact with urine, faeces, saliva or blood of infected rats; eating food or drinking water contaminated with urine, faeces, saliva or blood of infected rats; touching of floors, beddings and household materials contaminated with urine, faeces, saliva or blood of rats or an infected person; and person-to-person through contact with blood, urine, saliva, throat secretion or semen of an infected person”.
The Lassa fever virus is a familiar threat in Nigeria. In the week November 25 to December 1, 2019, eight new confirmed cases were reported in Ondo (six) and Edo (two) states, with two new deaths from Ondo. From January 1 to December 1, 2019, a total of 4,771 suspected cases were reported in 23 states. Of these, 793 were confirmed positive, 162 of which resulted in deaths.
“The rats in the kitchen are even bigger,” another patient added. “The first day I entered the kitchen was the day Yaba Left’s food began to irritate me. See, we, the patients, and the rats are eating the kitchen’s food together!”
MOSQUITOES AND EX-PATIENT’S BED SHEETS — WELCOME TO YABA LEFT

This announcement hit me below the belt. It was my second day at Yaba Left and I hadn’t seen anything encouraging. The previous night, the nurse on duty had told me to “manage this bedsheet for today” after I was checked into my ward. The bed sheet was originally coloured white but had become browned ostensibly by several years of overuse. The bed sheet smelled stale, clear proof it hadn’t been washed for days or weeks in the lead-up to the last patient’s exit.
On my 10th day at the ward, I summoned the courage to ask a senior nurse if my sheets would ever be changed. Her response was shocking.
“We can give you another one if you promise to wash it from time to time,” she said. “The problem is that when we send them to the laundry, white bed sheets suddenly become brownish.”
Yet all patients paid for laundry.
The bed sheet and rats weren’t the only oddities on my first night. The mosquitoes stung my legs mercilessly, no thanks to the overgrown lawn bordering the fence outside my ward and the Mrs. Adeniyi-purchased pyjamas that only stretched over a third of my legs. Consequently, my opening night was largely sleepless — and turbulent when I did manage to catch some sleep.
You can then imagine my consternation when I woke up in the morning to a breakfast that was two slices of yam, tasteless stew and a piece of fish half the size of my index finger. Afternoon was mashy rice — close to the kind of rice I once tweeted about — and beans. Evening was again eba, this time with vegetable and egusi that was not only insipid but also watery. I ate half and binned the rest. Trouble was already brewing but I didn’t know.
TROUBLE BREWING… A CIVIL, ANTI-FOOD PROTEST

Tests, tests, tests — and more tests!
I was soaking in Karl Meier’s ‘This House Has Fallen’, my most frequently-read book, the following morning, my third day at the ward, when the doctor overseeing Tolani Asuni announced that all patients needed to gather for a meeting. That, a two-time patient told me, was unusual for that hour of the day.
As we would later discover, some patients had written a protest letter to the authorities on behalf of the group, listing a number of grievances. Majority were minor but two were major: exit date and food. I at once dismissed the clamour for exit on the simple basis that nobody likes to lose their freedom, even though it is evident, in this case, that it must happen if they must be weaned off drugs. For drug patients, the psychiatric hospital is a glorified prison. They’re locked up in a ward. Whether they were brought in psychotic or conscious, they soon start feeling trapped in a matter of days. Yet, they can’t leave of their own volition; only the doctors or their parents or guardians can set them free — unless they want to escape, which has happened before. But I was quite happy the bad food had been brought up. Like others, I keenly awaited answers.
Dr. Ojo requested to know exactly those who wrote the letters. One was the Captain of the ward, one of the longest-serving patients. Soft-spoken and well-respected by the patients and even the nurses, he had been at the ward for close to three months and that was his second, possibly third, admission. The other, a lawyer, was a returnee-patient too. The lawyer was invited upfront to read the letter to the hearing of all. The session erupted in a cacophony of laughter when, while expressing displeasure with the food, he said: “The egusi soup is notoriously known to appear like a lagoon.”
There was hardly anyone who didn’t laugh but this was a very serious matter. For three reasons.
WHAT’S THE BIG DEAL ABOUT YABA LEFT’S FOOD?

The admission receipt… proof of the importance of feeding (half the total cost), and payment for laundry, which patients don’t always benefit from, and drugs, even though they weren’t prescribed for me.
Every drug patient pays a minimum of N120,000 for an initial two-month admission; N60,000 of that is for feeding. Technically, this means feeding is half the service rendered by Yaba Left. If it fails, therefore, the entire rehabilitation project is potentially as good as null. To put this in proper context, the next most expensive item after ‘feeding’ is ‘drugs’, at N20,000. And that’s one-third the cost of feeding!
Two, among the drugs taken by patients are Artane, which can cause dry mouth, and Thiamine, which can cause nausea. Therefore, patients on these drugs typically need their food tasty.
Three, drug patients are battling an addiction problem; if you take drugs away from their lips, you cannot afford to simultaneously take food away. Thiamine, for example, is a known appetite stimulant; you normally don’t give it to patients and starve them, which is technically what happens when they bin Yaba Left’s food.
And, finally, roughly a week before I was admitted, the hospital banned visitors from bringing in food for patients. The ban was the consequence of an ex-patient’s bad behaviour. The patient, Ife, had tried to import marijuana into the ward, via a Dundu Nation employee who folded six wraps of the weed among fried yams delicately packaged in a paper and foil. One patient told me arizona had been successfully imported and smoked at the ward a few times because of its discreet smell, but this time, the nurses intercepted the marijuana wraps at the point of entry, prompting uproar in the hospital. On learning of the development after a protocol breach that involved bypassing one or two doctors who could have smothered it, a thoroughly incensed Chief Medical Director, Dr. Oluyemisi Ogun, placed a ban on delivery of edible food to patients, save the ones brought by the two registered relatives who originally presented the patient for admission. Summary of the story, Yaba Left’s concoctions were the only edible food available to patients — and they were often terrible to behold, much less consume.
The protest letter of November 20 was laid to rest with a promise that things would improve, especially with regards to the food. They never did.
Editor’s Note: This is the first of a two-part series. Part II will be published on Friday.
This investigation was published with collaborative support from Cable Newspaper Journalism Foundation and Business Day.


Be the first to comment