The first patients to receive gene-editing treatments for inherited blood diseases will enter the new year free of agonising symptoms.
The experiments suggest that altering DNA could treat sickle cell disease (SCD) and beta thalassemia, conditions both caused by faulty genes that hamper the blood’s ability to carry oxygen.
The companies behind the trials said that a patient in the US with SCD had been well since July. A thalassemia patient in Germany had been free of symptoms for nine months. Previously she had 16 blood transfusions a year.
British patients could be offered similar experimental therapies next year. The treatment for both conditions involved a high-precision gene-editing tool called Crispr-Cas9. It was used to alter the DNA of some of the cells of Victoria Gray, 34, who has SCD. This caused her body to produce foetal haemoglobin, a substance not usually present after the age of six months.
Earlier work had shown that foetal haemoglobin effectively reversed the symptoms of SCD. Her doctor, Haydar Frangoul, said: “This approach is very exciting. If it is found to be safe and effective it can offer every patient with sickle cell disease a potential treatment.”
David Altshuler, chief scientific officer at Vertex, a company involved in the trials, said that it was “a scientific and medical milestone — the rapid and responsible evolution of Crispr technology from discovery of a technique suitable for a lab to a possible therapy with the potential to help patients with sickle cell disease.”
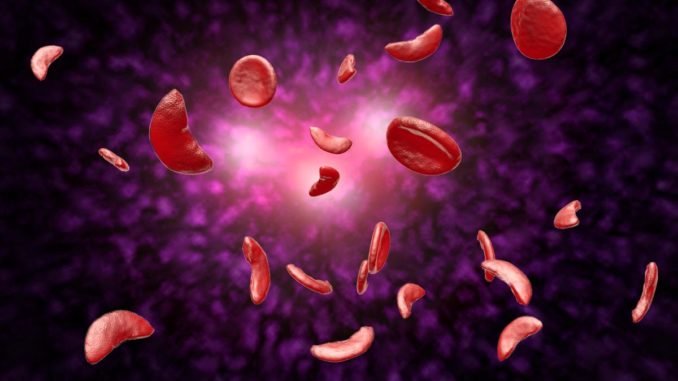
SCD is a genetic condition in which red blood cells, which should be circular, adopt a crescent shape and are sticky and rigid. They clog blood vessels and damage organs, causing agony. Some patients die in childhood.
Ms Gray was previously having seven painful episodes a year. Until now the only means of curing SCD involved a bone marrow transplant, which relies on a suitable donor and carries a risk of rejection and death.
The new treatment involved taking bone marrow stem cells from Ms Gray, who then had chemotherapy to kill her bone marrow. The extracted cells were edited using Crispr-Cas9, a tool at the forefront of genetics research.
It consists of a gene-cutting enzyme, primed with instructions that lead it to a particular part of a cell’s DNA. Once it arrives there it locks on to the string of DNA and snips out a portion, leaving the cell to repair the damage.
It was used to disable a gene that stops foetal haemoglobin being produced. Billions of Ms Gray’s blood-producing bone marrow cells were treated in this way before being infused back into her body.
A similar process was used for the beta thalassemia patient. Ciaran Lee, of University College Cork, said that previous studies involving individual cells had been highly promising. “What remains to be seen is if the stem cells corrected by Crispr can survive for the lifetime of the patient, providing a permanent cure, or if the effect is temporary.”
END

Be the first to comment